Lymphedema
Conditions
Overview
Lymphedema refers to tissue swelling caused by an accumulation of protein-rich fluid that's usually drained through the body's lymphatic system. It most commonly affects the arms or legs, but can also occur in the chest wall, abdomen, neck and genitals.
Lymph nodes are an important part of your lymphatic system. Lymphedema can be caused by cancer treatments that remove or damage your lymph nodes. Any type of problem that blocks the drainage of lymph fluid can cause lymphedema.
Severe cases of lymphedema can affect the ability to move the affected limb, increase the risks of skin infections and sepsis, and can lead to skin changes and breakdown. Treatment may include compression bandages, massage, compression stockings, sequential pneumatic pumping, careful skin care and, rarely, surgery to remove swollen tissue or to create new drainage routes.
Symptoms

Lymphedema signs and symptoms include:
- Swelling of part or all of the arm or leg, including fingers or toes
- A feeling of heaviness or tightness
- Restricted range of motion
- Recurring infections
- Hardening and thickening of the skin (fibrosis)
Signs and symptoms can range from mild to severe. Lymphedema caused by cancer treatment may not occur until months or years after treatment.
When to see a doctor
Make an appointment with your doctor if you notice persistent swelling in your arm or leg. If you've already been diagnosed with lymphedema, see your doctor if there is a sudden dramatic increase in the size of the involved limb.
Causes
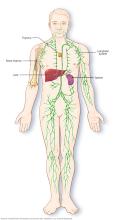
The lymphatic system is a network of vessels that carry protein-rich lymph fluid throughout the body. It's part of your immune system. Lymph nodes act as filters and contain cells that fight infection and cancer.
The lymph fluid is pushed through the lymph vessels by muscle contractions as you move through the tasks of your day and small pumps in the wall of the lymph vessels. Lymphedema occurs when the lymph vessels are not able to adequately drain lymph fluid, usually from an arm or leg.
The most common causes of lymphedema include:
- Cancer. If cancer cells block lymph vessels, lymphedema may result. For instance, a tumor growing near a lymph node or lymph vessel could enlarge enough to block the flow of the lymph fluid.
- Radiation treatment for cancer. Radiation can cause scarring and inflammation of lymph nodes or lymph vessels.
- Surgery. In cancer surgery, lymph nodes are often removed to see if the disease has spread. However, this doesn't always result in lymphedema.
- Parasites. In developing countries in the tropics, the most common cause of lymphedema is infection with threadlike worms that clog the lymph nodes.
Less commonly, lymphedema results from inherited conditions in which the lymphatic system doesn't develop properly.
Risk factors
Factors that may increase the risk of developing lymphedema include:
- Older age
- Excess weight or obesity
- Rheumatoid or psoriatic arthritis
Complications
Lymphedema complications may include:
- Skin infections (cellulitis). The trapped fluid provides fertile ground for germs, and the smallest injury to the arm or leg can be an entry point for infection. Affected skin appears swollen and red and is typically painful and warm to the touch. Your doctor may prescribe antibiotics to keep on hand so that you can start taking them immediately.
- Sepsis. Untreated cellulitis can spread into the bloodstream and trigger sepsis — a potentially life-threatening condition that occurs when the body's response to an infection damages its own tissues. Sepsis requires emergency medical treatment.
- Leakage through the skin. With severe swelling, the lymph fluid can drain through small breaks in the skin or cause blistering.
- Skin changes. In some people with very severe lymphedema, the skin of the affected limb can thicken and harden so it resembles the skin of an elephant.
- Cancer. A rare form of soft tissue cancer can result from the most-severe cases of untreated lymphedema.
Diagnosis
If you're at risk of lymphedema — for instance, if you've recently had cancer surgery involving your lymph nodes — your doctor may diagnose lymphedema based on your signs and symptoms.
If the cause of your lymphedema isn't as obvious, your doctor may order imaging tests to get a look at your lymph system. Tests may include:
- MRI scan. Using a magnetic field and radio waves, an MRI produces 3D, high-resolution images of the involved tissue.
- CT scan. This X-ray technique produces detailed, cross-sectional images of the body's structures. CT scans can reveal blockages in the lymphatic system.
- Ultrasound. This test uses sound waves to produce images of internal structures. It can help find obstructions within the lymphatic system and vascular system.
- Lymphoscintigraphy. During this test, the person is injected with a radioactive dye and then scanned by a machine. The resulting images show the dye moving through the lymph vessels, highlighting blockages.
Treatment
There's no cure for lymphedema. Treatment focuses on reducing the swelling and preventing complications.
Medications
Lymphedema greatly increases the risk of skin infections (cellulitis). Your doctor may prescribe antibiotics for you to keep on hand so that you can start taking them immediately once symptoms appear.
Therapy
Specialized lymphedema therapists can teach you about techniques and equipment that can help reduce lymphedema swelling. Examples include:
- Exercises. Gentle contraction of the muscles in the arm or leg can help move the excess fluid out of the swollen limb.
- Manual lymph drainage. Therapists trained in this massage-like technique use very light pressure to move the trapped fluid in the swollen limb toward an area with working lymph vessels. People should avoid manual lymph drainage if they have a skin infection, blood clots or active cancer in the affected limb.
- Compression bandages. Using low-stretch bandages to wrap the entire limb encourages lymph fluid to flow back toward the trunk of the body.
- Compression garments. Close-fitting elastic sleeves or stockings can compress the arm or leg to encourage lymph fluid drainage. These garments often require a prescription to ensure that the proper amount of compression is used. You may need to be measured by a professional to ensure proper fit.
- Sequential pneumatic compression. A sleeve worn over the affected arm or leg connects to a pump that intermittently inflates the sleeve, putting pressure on the limb and moving lymph fluid away from the fingers or toes.
- Lymph node transplant. Lymph nodes are taken from a different area of the body and then attached to the network of lymph vessels in the affected limb. Many people with early-stage lymphedema see good results from this surgery and can decrease the amount of compression needed.
- New drainage paths. Another option for early-stage lymphedema, this procedure creates new connections between the lymph network and blood vessels. The excess lymph fluid is then removed from the limb via blood vessels.
- Removal of fibrous tissue. In severe lymphedema, the soft tissues in the limb become fibrous and hardened. Removing some of this hardened tissue, often through liposuction, can improve the limb's function. In very severe cases, hardened tissue and skin may be removed with a scalpel.
Surgical and other procedures
Surgical treatment for lymphedema may include:
Lifestyle and home remedies
To reduce the risk of complications from lymphedema, avoid injuring the affected limb. Cuts, scrapes and burns can invite infection. Protect yourself from sharp objects. For example, shave with an electric razor, wear gloves when you garden or cook, and use a thimble when you sew.
Coping and support
It can be frustrating to know there's no cure for lymphedema. However, you can control some aspects of lymphedema. To help you cope, try to:
- Find out all you can about lymphedema. Knowing what lymphedema is and what causes it can help communication with the doctor or physical therapist.
- Take care of the affected limb. Clean your skin daily, looking over every inch of the affected limb for signs of trouble, such as cracks and cuts. Apply lotion to prevent dry skin.
- Take care of your whole body. Eat a diet rich in fruits and vegetables. Exercise daily, if you can. Reduce stress. Try to get enough sleep. Taking care of your body gives you more energy and encourages healing.
- Get support from others with lymphedema. Whether you attend support group meetings in your community or participate in online message boards, it helps to talk to people facing similar difficulties.
Preparing for an appointment
Here's some information to help you get ready for the appointment with your doctor.
What you can do
List the following:
- Your symptoms, including any that may seem unrelated to the reason for which you scheduled the appointment
- Key personal information, including major illnesses or trauma, cancer treatments or recent life changes
- Medications, vitamins and supplements you take
- Questions to ask the doctor
For lymphedema, some basic questions to ask the doctor include:
- What's the likeliest cause of this swelling?
- Could there be another cause?
- What tests do I need? Do these tests require special preparation?
- Is the swelling temporary or long lasting?
- What's the treatment for lymphedema?
- Are there alternatives to the approach you're suggesting?
- Are there medications to ease the swelling?
- I have other health conditions. How can I best manage them together?
- Do I need to restrict my diet or activities?
- Do you have brochures or other printed material that I can take? What websites do you recommend?
Don't hesitate to ask other questions, as well.
What to expect from the doctor
Your doctor is likely to ask you a number of questions, such as:
- When did the swelling begin?
- Did anything precede the swelling, such as surgery, trauma, radiation therapy or new medications?
- Do you have other signs or symptoms?
- Has the swelling been continuous or occasional?
- Does anything seem to make the swelling better?
- Does anything seem to worsen the symptoms?
- What have you tried to treat the edema, and how did it work?
What you can do in the meantime
Keep the swollen limb elevated as much as possible and protect your skin from injury. The swelling from lymphedema might dull pain from an injury or burn, so don't use heating pads on the affected limb. Moisturize your skin daily.
© 1998-2025 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
